Understanding Trauma-Informed Care
When it comes down to trauma-informed care in crisis response, it’s important to really get what makes this approach tick, and why it’s so essential for folks who’ve been through rough times.
Principles of Trauma-Informed Care
Trauma-informed care (TIC) boils down to bustin’ up the cycle of trauma and giving folks a boost where they feel safe, powerful, and worthy again. It’s like building someone up with the basics:
- Safety: Create a cozy, secure spot where folks can chill and heal.
- Trustworthiness and Transparency: Say what you mean, mean what you say, and never leave ’em guessing.
- Peer Support and Mutual Self-Help: Because sometimes, sharing is caring. Lean on each other.
- Collaboration and Mutuality: Team up with folks to help them take charge of their journey.
- Empowerment, Voice, and Choice: Let them call the shots when it comes to their own care.
- Cultural, Historical, and Gender Issues: Everybody’s got different stories. Respect and embrace them all.
These principles show you the nuts and bolts of creating a space where folks can get back on their feet and come out even stronger after going through trauma.
Importance of Trauma-Informed Approach
Trauma-informed care gets that the magic of healing happens best when relationships are built on trust and empowerment. It’s all about joining hands in shared decision-making and genuine partnerships. Service providers that jump on the trauma-informed bandwagon can really meet people where they are, catering support to their special strengths and quirks.
Taking up trauma-informed care in mental health services isn’t just crucial—it’s a game-changer. It can level up the care quality and drop rates of restraint and seclusion (NCBI). Sure, it might take some time and resources to get going, but the payoff in terms of better wellness and recovery makes it totally worth it.
By getting and living the trauma-informed care vibe, organizations and individuals can open their doors to healing, build up resilience, and make the world a more caring place for those who’ve faced the storm.
Application in Healthcare Settings
Taking a deep dive into trauma-informed care (TIC) within healthcare settings unearths some pretty striking effects, both on those receiving the care and on the folks providing it. By bringing trauma-informed methods into the mix, these environments are reporting successes like enhanced patient well-being and more teamwork and support among staff.
Implementing Trauma-Informed Care
Working trauma-informed care into healthcare, especially in the good ole USA (22 out of 27 cases show it’s making waves!) is a big step towards treating folks who’ve been through the wringer with genuine compassion. By putting trauma-informed ideas into play, healthcare pros can craft a space that feels both welcoming and safe, tuning into what each patient uniquely needs from them.
For healthcare spots to properly embrace this, they’ve gotta get some serious training to understand the ins and outs of trauma. This learning process aims to help staff better recognize trauma’s signs and provide care that’s compassionate, smart, and directly meets the patient’s needs.
Impact on Service Users and Staff
Rolling out trauma-informed care has sparked a variety of positive shifts for patients and healthcare workers alike. These changes have bolstered survivors’ mental and emotional health, ramped up staff skills, and shrunk the use of measures like seclusion and restraint, according to findings from the National Center for Biotechnology Information. None of it’s guesswork: trauma-smart strategies like the Six Core Strategies have cut down on seclusion and physical restraints in hospitals, especially among younger folks. Facilities diving into these practices note less need for such tough-on-the-body approaches, pointing to a more compassionate care model.
Giving trauma-informed care the front seat makes healthcare not only about treatment but about understanding and nurturing a culture that soaks up empathy and healing for everyone crossing its path—patients and providers included. Tweaking the framework into a trauma-smart one doesn’t just uplift the care given but also builds an all-around supportive vibe that honors everyone’s dignity and health.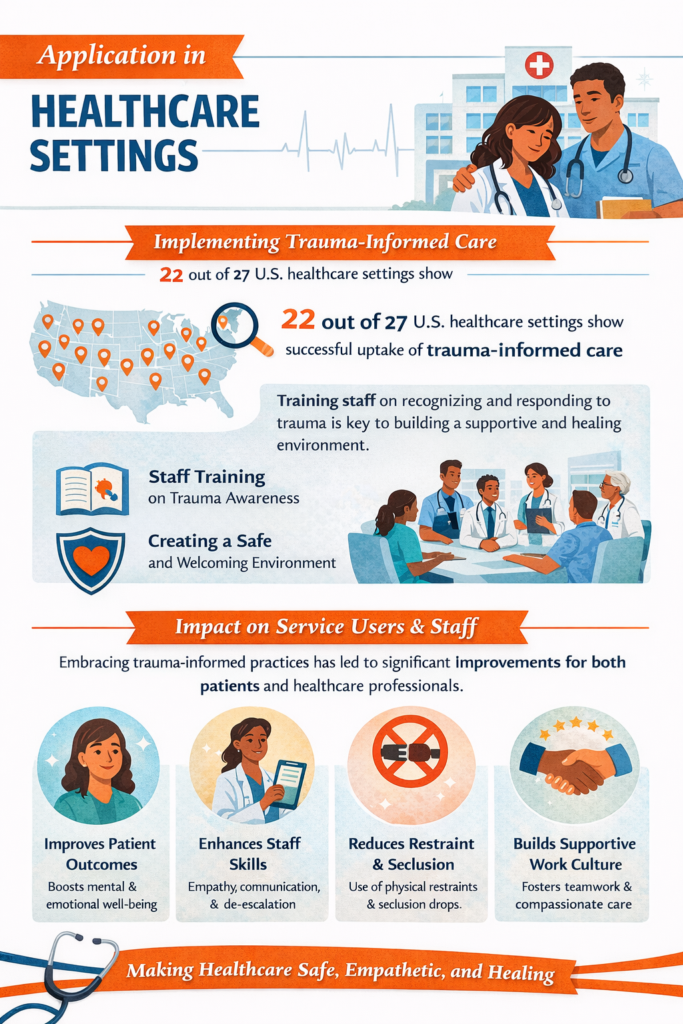
Trauma and Mental Health Services
These days, when it comes to mental health, knowing how to work with trauma-informed care is like having a map to a hidden treasure. It’s a big deal, offering a real boost to folks battling trauma. Ever wondered why trauma seems to pop up so much in mental health settings, and how lowering restraint and seclusion can make life better for everyone? Here’s the skinny:
Trauma in Mental Health Settings
You don’t have to dig too deep to see that a lot of folks in mental health care have seen some tough times. Especially in places like the U.S., studies shout out that trauma really lingers in these environments (NCBI). It’s key to get how trauma changes someone’s headspace so we can tweak the help we give.
With trauma-informed care, the game plan is simple: make a warm and welcoming space that doesn’t just see the trauma, but really “gets” how it plays out in a person’s life story. Mental health warriors, this is your chance to build trust, give folks a bit of their mojo back, and get them on the healing journey.
Decreasing Restraint and Seclusion
Now, restraint and seclusion. Once upon a time, these were the go-tos for “managing” behavior. But, they can slap more hurt on people who’ve already seen enough, and that ain’t right. Research tells us that bringing trauma-informed techniques onboard actually leads to less of these harsh measures (NCBI).
So, what’s the plan? Focus on stopping trouble before it starts. Make spaces that get what trauma’s about, use less harsh alternatives, and train staff on how to calm a boiling pot without blowing it up. This way, we’re growing environments full of safety, respect, and a whole lot of understanding. It’s a win for everyone—those who need the care feel less attacked, and staff folks get to work with empathy and real heart
To pull this off right, mental health teams should put a laser focus on training staff in trauma care. Arm them with knowledge and tools, and watch how services get a serious glow-up. It’s all about paving the path to recovery and making a killer support system for anyone looking for help.
Factors Influencing Implementation
Getting trauma-informed care going in crisis response isn’t just a matter of flipping a switch. It’s like baking a cake—you gotta have the right ingredients and make sure you’ve got the right conditions. Here’s what makes it work and what might put a wrench in the works.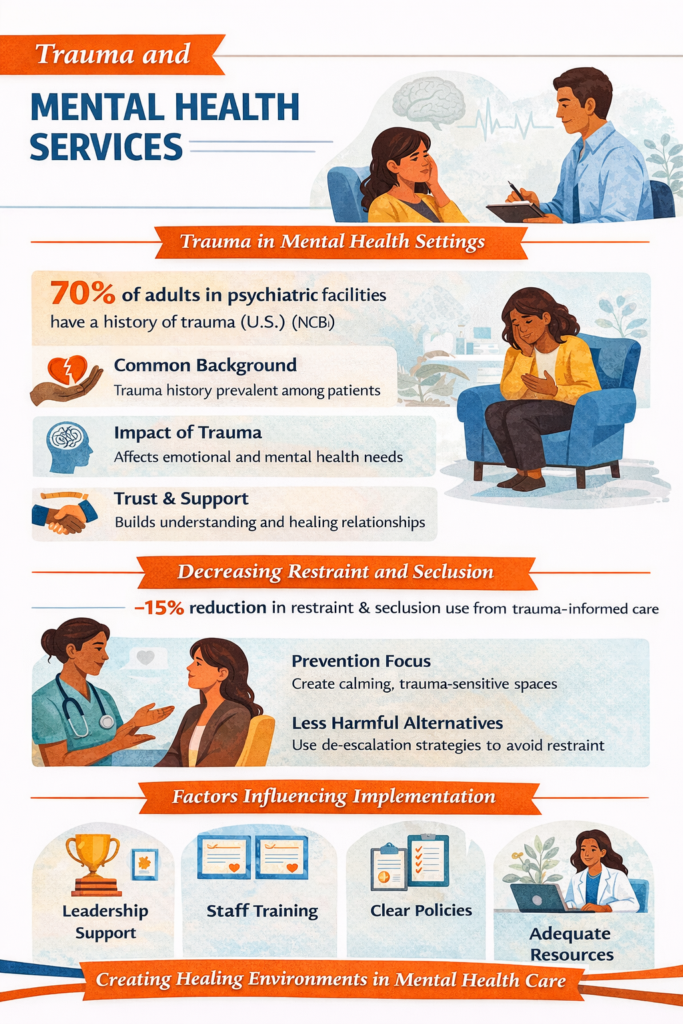
Successful Implementation Factors
Getting trauma-informed care to actually work in crisis moments takes a mix of strategy and good vibes in the workplace. Here’s the stuff that helps:
- Leadership Engagement: You need leaders who are all-in and not just nodding along. When the people at the top walk the walk, it sets the tone and makes everyone else pay attention. They’re the ones who say, “This is important, and we mean it.”
- Financial and Staffing Resources: Money talks, right? If you don’t have enough dough or enough folks to help, it’s tough to keep these programs alive and kicking. Solid funding means you can keep up training and services without hitting the brakes.
- Policy and Procedure Changes: Shuffling the rulebook a bit is part of the game. Making sure every policy includes taking trauma into account is key. That way, you’re not just slapping on a band-aid but making sure every step fits with the plan.
- Flexible Training: Crisis workers need training that bends with the roads they’re traveling. You don’t just chuck ’em in a classroom once. It’s ongoing, focusing on understanding trauma, building resilience, and nailing those communication skills.
- Service User Feedback: Listening to those in the thick of it—yep, the people you’re helping—keeps things real. Their insights stop things from getting too textbook and make sure you’re meeting real needs.
Barriers to Implementation
Plenty of things can trip you up when putting trauma-informed care into action. Here’s what could slow the roll:
- Resistance to Change: Nobody likes change, right? Getting folks on board with new methods can be as tough as dragging a mule through mud. You’ve gotta spend time explaining, cheering folks on, and being there while things shift.
- Limited Resources: Money trouble and not enough hands on deck can stall everything. Without the goods to keep going, even the best plans can fall apart.
- Lack of Training: If crisis responders aren’t up to speed, that’s a snag. Gaps in what they know could mean trauma-informed care ends up being a well-meant sticker instead of something that really sticks.
- Organizational Culture: Some places just aren’t set up for change—they might be stuck in the past where trauma care doesn’t fit. It takes some serious culture rewol to swaying minds and getting on the right track.
Sorting through these hurdles and getting creative with solutions gives crisis responders a better shot at making trauma-informed care a real thing. Balancing out what works and what doesn’t means everyone—those helping and those being helped—gets something good from the deal.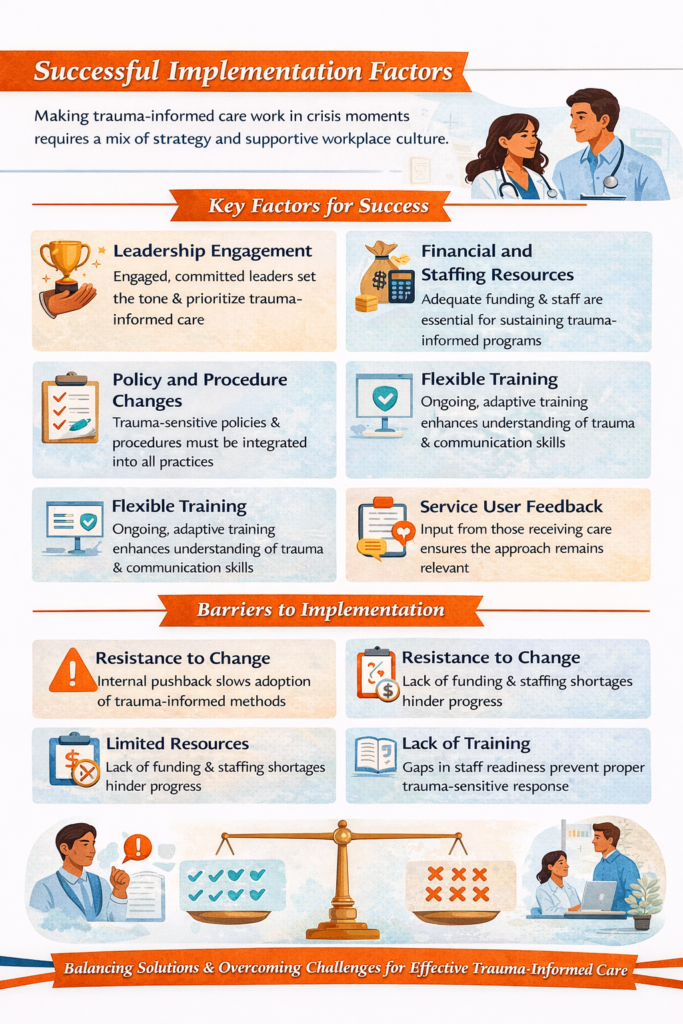
Trauma-Informed Language in Public Health
Okay, let’s chat about trauma-informed care in crisis situations. Imagine a friendly voice in your head saying, “Aw, there, there…it’s going to be okay.” That’s the vibe we’re aiming for here, crafting a cozy spot for folks who’ve been through the wringer. Using the right words can be like wrapping someone in a warm, reassuring blanket—they feel safe, heard, and not alone in their journey.
Integrating Trauma-Informed Principles
According to the clever minds over at the Substance Abuse and Mental Health Services Administration (SAMSHA), there are some basics to keep in mind: things like safety, honesty, and giving people a say in their own lives. It’s like mixing a recipe for trust that’s been handed down through generations. Don’t forget to add a sprinkle of cultural respect—everyone’s story matters.
When public health folks get the hang of these trauma-informed ideas, they’re not just ticking boxes. They’re genuinely valuing and lifting up folks who’ve been through tough times. It’s all about creating a space where healing beats trauma every time.
Benefits for Public Health Professionals
Switching gears to the perks: speaking the trauma-informed lingo means health pros have a better shot at understanding what folks who’ve faced tough stuff are going through. It’s like wearing empathy glasses—they see challenges clearer and can help more effectively.
Plus, getting this knowledge into education and training for the upcoming batch of health professionals is key. It’s like giving them a starter pack full of golden rules to follow from day one. No one’s going to be left feeling unseen or unheard—they’ll know how to tackle sensitive issues without making anyone relive their nightmares.
Keeping trauma-informed language in our toolkit isn’t just about creating a nurturing environment—though that’s a big plus. It’s also about helping communities bounce back stronger than ever. Less of a ‘one-size-fits-all’ approach, more of a ‘we’ve got your back’ way of doing things. And that’s something that makes everyone breathe a little easier.
Trauma-Informed Approaches in Practice
Ever wonder how real-life stories shed light on trauma-informed care in crisis situations? Peeking into actual cases and seeing the good they bring can really shape how we handle things better moving forward. Let’s hop into some real examples and dig into takeaways that’ll make this all-in-one practice run smoother.
Case Studies and Positive Outcomes
Hospitalized Youth Mental Health Program
Have you seen the magic of trauma-informed methods? There was this program that really nailed it by cutting back on seclusion and restraint for kids in hospitals. We’re talkin’ real change, folks! These strategies worked wonders, showing how to tackle mental health challenges in settings that need it the most (NCBI).
| Program Outcome | Result |
|---|---|
| Reduction in Seclusion and Restraints | Huge drop |
| Positive Impact on Youth | Mental health boosted |
Psychiatric Residential Treatment Facilities
Folks in the Midwest of the U.S. jumped on a trauma-informed approach at psychiatric places housing trauma-hit youngsters. They saw a big fall in using physical restraints. This showed how going with trauma-informed care does wonders (NCBI).
| Facility | Outcome |
|---|---|
| Reduction in Physical Restraints | Major drop |
| Improvement in Patient Care | Better treatment results |

Lessons Learned for Future Integration
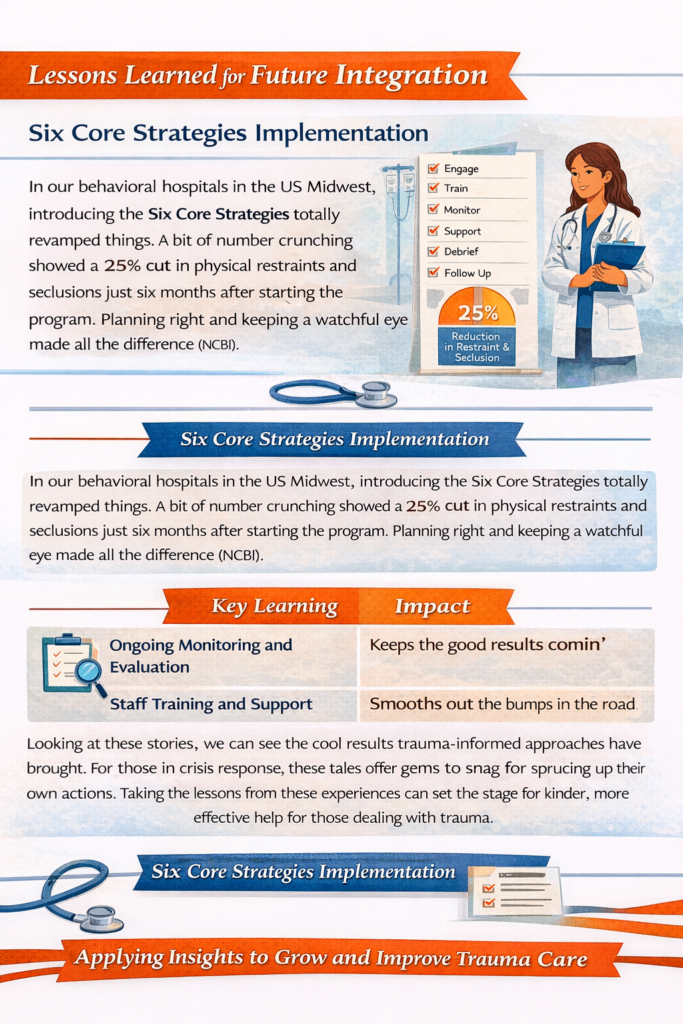
Six Core Strategies Implementation
In our behavioral hospitals in the US Midwest, introducing the Six Core Strategies totally revamped things. A bit of number crunching showed a 25% cut in physical restraints and seclusions just six months after starting the program. Planning right and keeping a watchful eye made all the difference (NCBI).
| Key Learning | Impact |
|---|---|
| Ongoing Monitoring and Evaluation | Keeps the good results comin’ |
| Staff Training and Support | Smooths out the bumps in the road |
Looking at these stories, we can see the cool results trauma-informed approaches have brought. For those in crisis response, these tales offer gems to snag for sprucing up their own actions. Taking the lessons from these experiences can set the stage for kinder, more effective help for those dealing with trauma.